Recommendations for laboratory testing of UK patients with acute myeloid leukaemia
Nick Telford, Chris Wragg, Richard Dillon and Sylvie Freeman contributed equally to this work.
METHODOLOGY
This Good Practice Paper was compiled according to the BSH process (https://b-s-h.org.uk/media/19922/bsh-guidance-development-process-july-2021.pdf). The British Society for Haematology (BSH) produces Good Practice Papers to recommend good practice in areas where there is a limited evidence base but for which a degree of consensus or uniformity is likely to be beneficial to patient care. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) nomenclature was used to evaluate levels of evidence and to assess the strength of recommendations. The GRADE criteria can be found at http://www.gradeworkinggroup.org.
REVIEW OF THE MANUSCRIPT
Review of the manuscript was performed by the British Society for Haematology (BSH) Guidelines Committee and the Haematology Oncology sounding board of BSH. It was also on the members section of the BSH website for comment. It has also been reviewed by National Genomic Medicine Service and the Association for Clinical Genomic Science (genetics sections consultation for 4 weeks from 20/09/2021) and the NCRI AML working party. These organisations do not necessarily approve or endorse the contents.
INTRODUCTION
Making a diagnosis of acute myeloid leukaemia (AML) requires a multi-faceted approach bringing together clinical features of patient presentation with laboratory investigations encompassing morphological, immunophenotypic and genetic evaluation of blood, bone marrow and, when appropriate, cerebrospinal fluid (CSF). Recent years have seen updates in disease classification and risk stratification, the rapid incorporation of novel laboratory techniques into routine practice and significant changes in treatment algorithms brought about by the approval of a range of new therapeutic agents.
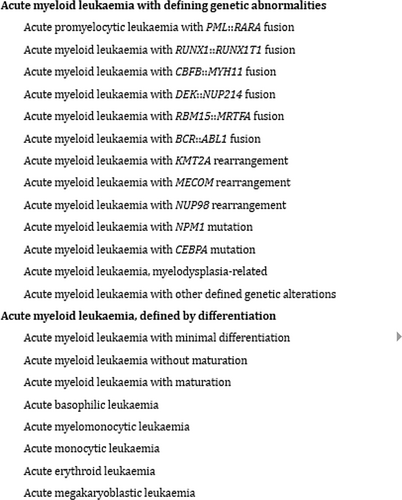
The revised 2022 World Health Organisation (WHO) Classification1 subdivides AML into two categories: AML with defining genetic abnormalities (DGA) and AML defined by differentiation (see Appendix A). A key change is the elimination of the 20% blast requirement for AML types with DGA, with the exception of BCR::ABL1 and CEBPA mutation. There is also the introduction of ‘AML with other defined genetic alterations’ which would incorporate new and/or uncommon AML subtypes that may be identified in the future. The classification of AML has also been updated separately by the International Consensus Classification (ICC).2
Increased emphasis is placed on genetic factors by both classifications, although morphological assessment retains importance in initial diagnosis, guiding the application of further tests and remains crucial in the emergency identification of acute promyelocytic leukaemia (APL). European Leukaemia Net (ELN) recommendations4 were also updated in 20223 and represent the current standard-of-care for AML patient risk stratification (see Appendix B), mandating multi-platform genetic evaluation that incorporates cytogenetic and molecular testing, including addition of next-generation sequencing (NGS) analysis to detect prognostically-relevant entities such as AML with mutations in CEBPA and TP53, and those mutations associated with secondary AML (i.e. ASXL1, BCOR, EZH2, RUNX1, SF3B1, SRSF2, STAG2, U2AF1, and ZRSR2).
Since 2018, ten new drugs have been approved for use in AML by the US Food and Drug Administration (FDA), with six of these now approved by the National Institute for Health and Care Excellence (NICE) (summarised in Table 1). Three of these NICE-approved agents have now been incorporated into frontline intensive treatment algorithms for newly diagnosed ‘non-APL’ AML, emphasising the need for timely turnaround of FLT3 mutation testing (midostaurin), for accurate identification of AML with myelodysplasia-related cytogenetic abnormalities (CPX-351) and of CD33-positive AML with non-adverse risk karyotype (gemtuzumab ozogamicin; GO). Greater appreciation of the prognostic associations of TP53 mutations (and interaction with cytogenetic findings) makes their early identification increasingly relevant to treatment decisions in individual patients.4, 5
| Drug | Drug class | Approved indicationa | NICE | FDA | EMEA |
|---|---|---|---|---|---|
| Midostaurin | Multi-targeted kinase inhibitor | Newly diagnosed FLT3-mutated AML (in combination with intensive induction and consolidation chemotherapy, and alone after complete response as maintenance therapy) |
Recommended (June 2018) |
||
| Arsenic trioxide | Inorganic compound |
Acute promyelocytic leukaemia (APL). 1. Untreated, low-to-intermediate risk disease (WBC < 10x109/ml) when given with all-trans-retinoic acid (ATRA) or 2.Relapsed or refractory disease, after a retinoid and chemotherapy. |
Recommended (June 2018) |
ü | |
| Gemtuzumab ozogamicin | Anti-CD33 antibody-drug conjugate | Untreated de novo CD33-positive AML in adults. Cytogenetics favourable, intermediate, failed or not yet available |
Recommended (Oct 2018) |
||
| CPX-351 | Cytotoxic (liposomal daunorubicin/cytarabine) | Untreated therapy-related AML or AML with myelodysplasia-related changes in adults. |
Recommended (Nov 2018) |
||
| Gilteritinib | FLT3 inhibitor | Relapsed or refractory FLT3-mutation-positive AML in adults |
Recommended (Aug 2020) |
||
| Enasidenib | IDH2 inhibitor | Relapsed/refractory IDH-2 mutated AML | Not assessed6 | ||
| Ivosidenib | IDH1 inhibitor | Relapsed/refractory IDH- 1 mutated AML | Not assessed7 | ||
| Venetoclax | BCL2 inhibitor | Newly diagnosed AML (in combination with azacitidine) for patients unsuitable for intensive chemotherapy |
Recommended (Feb 2022) |
||
| Glasdegib | Smoothened inhibitor | Newly diagnosed AML (in combination with low dose cytarabine) for patients unsuitable for intensive chemotherapy | Not assessed8 | ||
| CC-486 | Oral hypomethylating agent | As maintenance treatment for adults who have achieved CR/CRi following intensive induction chemotherapy who are not proceeding to haematopoietic SCT | Under assessment9 |
- Abbreviations: EMEA, European Medicines Agency; NICE, National Institute for Health and Care Excellence; FDA, US Food and Drug Administration.
- a Where the drug is NICE-approved, the stated indication is as per the terms of the NICE guidance. Where the drug is not yet NICE approved or has not been assessed by NICE, the stated indication is as per terms of US FDA approval.
Differing rates of adoption of novel diagnostic techniques and regional variations in laboratory practice have resulted in significant heterogeneity, both in access to investigations and in laboratory turnaround times. In this BSH Good Practice paper we make recommendations on best practice in the laboratory evaluation of patients with AML at the points of initial diagnosis and relapse, including guidance on laboratory turnaround times, that allow prompt access to genetically- and disease subgroup-defined approved therapeutic agents across the UK.
Sampling considerations
Patients suspected to have AML should have a bone marrow (BM) examination (aspirate and trephine biopsy). For patients with a high white blood cell count at presentation, diagnostic workup may be performed on the peripheral blood (PB) in lieu of a BM examination, and this may also be a suitable approach for the older/frail patient or when best supportive care is likely to be the most appropriate treatment option. Specific sampling requirements for tests are listed in Table 2. Other important considerations at the time of diagnosis are: (1) samples for trials and/or biobanking, (2) samples to allow definition of a flow cytometric or molecular measurable (minimal) residual disease (MRD) marker for future monitoring for patients treated outside clinical trials [storage of DNA and RNA is considered mandatory and a sample to assess leukaemia-associated immunophenotype (LAIP) is strongly recommended] (3) adequate consent and (4) the logistics of transport to laboratories. Integrated reporting of morphology, immunophenotyping and genetics on a sample by a Specialist Integrated Haematological Malignancy Diagnostic Service (SIHMDS) was recommended by NICE Improving Outcomes Guidance in 2016 (https://www.nice.org.uk/guidance/ng47). Integrated reports should specify the classification used in making the diagnosis of AML.
| Test | Sample requirements | |
|---|---|---|
| Morphology (PB & BM) | Diagnosis, follow-up and suspected relapse |
|
| Trephine biopsy | Diagnosis and suspected relapse |
|
| Flow cytometry | Diagnosis, follow-up (specified time points) and suspected relapse—key sample characteristics |
|
| Diagnosis or suspected relapse |
BM: 2–5 ml in EDTA tube PB: 10–20 ml in EDTA tube |
|
| Follow-up including for MRD assessment | BM: 2–5 ml in EDTA tube | |
| CSF for suspected CNS involvement |
|
|
| Genetics | Cytogenetics and FISH |
BM: in heparinised Transport Medium (supplied by Cytogenetics laboratory) or lithium heparin tube Should reach the laboratory within 24 h |
|
Molecular rapid single target testing Myeloid gene panel analysis |
BM: 2–3 ml in EDTA tube and/or PB: 4 ml in EDTA tube |
|
| Molecular fusion detection and MRD assessment |
BM: 5 ml in EDTA tube and/or PB: 20 ml in EDTA tube Should reach the laboratory within 48 h |
|
- Abbreviations: BM, bone marrow; CNS, Central Nervous System; CSF, cerebrospinal fluid; EDTA, Ethylenediaminetetraaceticacid; FISH, Fluorescence in situ hybridisation; MRD, measurable (minimal) residual disease; PB, peripheral blood; RNA, Ribonucleic acid.
Morphology
In the 2022 revision of the WHO AML classification, a BM or PB blast count of ≥20% is required only for the diagnosis of AML without defining genetic abnormalities (DGA) (Appendix A). For AML with DGA, a blast count of >20% is not required and a specific blast cut off has not been set, with increased emphasis on correlation between morphologic findings and molecular genetic studies. Similarly, the International Consensus Classification of AML (ICC) presented in 2022 (EHA reference) has suggested a lower blast count of ≥10% for AML with DGA, and proposes the category of MDS/AML for patients with 10%–19% blasts in PB or BM with subcategories of AML with MDS related gene mutations and AML with MDS related cytogenetic abnormalities in patients without DGA.
The new 2022 WHO classification has replaced the category of AML with myelodysplasia-related changes (AML-MRC) with AML-Myelodysplasia Related (AML-MR) and its diagnostic criteria are updated (see Endnote). Key changes include removal of morphology alone to make a diagnosis of AML-MR, updating the cytogenetic criteria and introducing the mutation-based diagnosis of AML-MR. AML transformed from MDS or MDS/MPN continues to be included in AML-MR in view of the broader unifying biologic features.
Morphologically, myeloblasts, monoblasts and megakaryoblasts are included in the blast count. In AML with monocytic or myelomonocytic differentiation, monoblasts and promonocytes, but not abnormal monocytes, are counted as blast equivalents. Diagnostic criteria for Acute Erythroid Leukaemia (AEL) include erythroid predominance, usually >80% of BM elements, of which >30% are proerythrobalsts.
Endnote: Access to drugs in the treatment of AML currently approved in the UK are based on previous classification and disease definitions. Hence relevant funding approval criteria should be referred to when accessing these drugs.
Morphology recommendations
- Bone marrow aspirate and trephine biopsy should be performed and at least 200 nucleated cells examined to make a diagnosis of AML.
- Communicating morphological findings rapidly to specialised laboratory personnel is important to aid further testing, especially if suspecting APL or core-binding factor (CBF) AML - cases with t(8;21), t(16;16) or inv(16).
FLOW CYTOMETRY
Immunophenotypic profiling by multiparametric flow cytometry (MFC) is essential at diagnosis, for remission assessment and if relapse is suspected. Testing of CSF is required when CNS involvement is suspected. Eight-colour MFC panels are standard, although it is anticipated that 10-colour panels will become routine in the next few years due to the newer clinical cytometers now available.
MFC-MRD in AML applied to remission BMs provides additional prognostic information after induction chemotherapy and pre-transplant; it may also be informative at other time-points. SIHMDS are recommended to have a named reference laboratory for MFC-MRD testing. This may require additional standard operating procedures (SOPs) for send away tests.
Sample requirements for MFC tests are according to Table 2.
Turnaround times
- same working day when received before 3:30 pm
- processed same day or next morning with results available <2–3 working days from sample receipt.
Diagnostic panels
- an acute leukaemia screen (such as the Euroflow ALOT combination)10 to confirm leukaemic blasts and allow lineage assessment
- followed immediately by an AML-specific panel if appropriate
- extended secondary testing may be required to diagnose blastic plasmacytoid dendritic cell neoplasm (BPDCN)11 or ambiguous leukaemias or acute megakaryoblastic leukaemia (Table 3).
| Antibody markers | Comments | |
|---|---|---|
| Acute megakaryoblastic leukaemia | Extended testing includes CD41, CD61, CD36, CD9 may also be helpful |
|
| Blastic plasmacytoid dendritic neoplasm (BPDCN) | Extended testing includes CD123, CD4, CD56 | |
| t(8;21) | CD19, CD56, CD34, CD33 | Blast immunophenotype:
|
| t(15;17) | CD117, CD34, CD11b, HLA-DR, CD33, CD13 | Promyelocyte immunophenotype
|
| MRD panel | CD45 CD33 CD13 CD34 CD117 HLA-DR CD56 CD7 |
|
- Abbreviation: MRD, measurable (minimal) residual disease.
- a Blasts of NPM1 mutated AML may also be negative for CD34, HLA-DR and CD11b and positive for CD117 but typically have lower side scatter and may have monocytic component.
Myeloperoxidase positivity for myeloid lineage assignment can be defined as ≥20% of acute leukaemic cells exceeding a lymphocyte-based threshold.12
APL and t(8;21)/RUNX1::RUNX1T1 AML have typical blast immunophenotypes (Table 3); prompt reporting of these in conjunction with morphology can expedite confirmatory genetic tests.
Characterisation of diagnostic leukaemic aberrant phenotypes informs further monitoring. This requires diagnostic as well as follow-up AML samples to be tested by an AML MRD minimum marker set (Table 3). Therefore, diagnostic samples may need to be routinely sent to the reference MFC-MRD laboratory.
Treatment authorisation for GO requires CD33 positivity. All AML diagnostic and relapse reports should include clear information on whether blasts are CD33 positive. There is heterogeneity in the clinical effectiveness of GO that, in part, correlates with higher CD33 expression levels, but GO can be effective in patients with partial or weak blast CD33 positivity as observed for CBF AMLs.13 MFC laboratories will have validated fluorescent thresholds for quantifying % CD33-positive blasts and maintain a satisfactory performance for this marker in an external quality assurance scheme such as the UK NEQAS Leukaemia Immunophenotyping Part 1. Expression of other markers may also be a requirement for future immunotherapy indications such as CD123 for tagraxofusp as first line treatment in BPDCN (FDA and EMA approved).14, 15
Flow cytometric remission and MRD assessment
BMs may be inadequate or suboptimal for assessment of remission or MRD; this should be stated in the report, along with the cause (poor cell viability/haemodilution/insufficient leukocytes). Other critical report information includes blast percentage, markers defining the blast population and the denominator for blast percentage (leukocytes or nucleated cells).
In some cases, flow cytometric and morphological results will be discrepant for remission status; potential contributing technical and sampling factors should be considered as part of integrated SIHMDS reporting. If patients are refractory by morphology but have an MFC-MRD negative test, the latter appears to be more reliable for prognosis.16-19
MFC-MRD assessment should be performed with a qualified assay according to ELN guidelines,20, 21 and is best achieved in a laboratory with specialist expertise in AML MFC-MRD that coordinates with genetic AML MRD laboratories for guidance on the most appropriate MRD test and result interpretation. The prognostic value of MFC-MRD may be reduced by methodological variability such as in instrument settings, panels and analysis.22, 23
Flow cytometry recommendations
- Flow cytometric analyses are critical for diagnosis and remission assessment and require rapid reporting.
- Diagnostic reports should record whether AML cells are CD33 positive.
- Diagnostic AML subtyping by flow cytometry should include consideration of blastic plasmacytoid dendritic cell neoplasm (BPDCN)
- For flow cytometric MRD monitoring, a diagnostic sample is preferred to identify trackable MRD targets
GENETICS
Comprehensive genetic profiling, comprising cytogenetic and molecular genetic testing, is integral to the diagnosis and classification of AML (Table 4).25-27 Detection of disease-specific abnormalities supports accurate diagnosis and yields prognostic information for risk stratification and is critical at diagnosis and at relapse. If a case is discovered to be high risk MDS (e.g., high blast count), then at the time of initial request or subsequently, testing should be undertaken as per the AML pathway.
| Test name | TAT (days) |
|---|---|
| FLT3 ITDa | 3 |
| NPM1 exon 11 | 3 |
| FLT3 TKD hotspota | 3 |
| FISH/PCR or Karyotype CBFB::MYH11 [inv16] | 3 |
| FISH/PCR or Karyotype RUNX1::RUNX1T1 [t(8;21)] | 3 |
| AML Karyotypea,b | 7 |
| KMT2A::R FISH | 14 |
| AML NGS Panela,c | 14 |
| WGS Germline and Tumourd | 42 |
- Abbreviation: TAT, Turnaround time.
- a It is essential that these tests are repeated at relapse. Other tests may need to be repeated at relapse, depending on the clinical situation.
- b Cytogenetically cryptic CBF should be excluded where diagnostic suspicion persists.
- c NGS panel should include as a minimum, ASXL1, BCOR, EZH2, RUNX1, SF3B1, SRSF2, STAG2, U2AF1, ZRSR2, TP53, FLT3, IDH1, IDH2, DNMT3a and WT1.
- d May be used to supplement standard-of-care studies, and considered in patients being investigated for germline predisposition.
Accurate and rapid genetic characterisation allows timely deployment of specific therapeutic interventions; either according to subtypes defined by cytogenetics (e.g., CBF AML and AML with myelodysplasia-related cytogenetic abnormalities) or to specific mutations (e.g., FLT3 and IDH1/2). Identification of characteristic genetic lesions also identifies patients suitable for molecular monitoring of residual disease. Storage of appropriate material for further molecular and cytogenetic studies is essential in all patients, and cell suspension, DNA and RNA should be stored, with appropriate written informed consent in place, at diagnosis and relapse where possible.
Cytogenetic testing is mandatory at both diagnosis and relapse. Conventional karyotyping may be supplemented by rapid fluorescence in situ hybridisation (FISH) testing to promptly identify cardinal lesions associated with various AML subtypes, however in the absence of a diagnostic finding, FISH must always be supplemented by a rapid karyotype. In the event of karyotyping failure, SNP Microarray or FISH for del(5q), del(7q) and monosomy 7 and del17p (TP53) will detect a significant proportion of myelodysplasia-related abnormalities, however, it should be noted that multiple rare abnormalities and complex karyotype may be missed when using FISH alone.
Subsequent monitoring by FISH or karyotyping is not routinely recommended, however may add value in clarifying atypical or discordant results of other testing modalities or where progression or relapse are suspected.
PML::RARA testing is not mandatory for all cases of AML, but must be rapidly initiated in selected cases where the results of other testing (e.g., morphology) provide a high index of suspicion of APL. Where indicated, PML::RARA testing must be available within 24 h. It is important to note that a small proportion of rearrangements can occur which are both chromosomally cryptic and also undetected by FISH analysis. Molecular characterisation should be offered where clinical suspicion persists, for the identification of cryptic abnormalities in difficult cases. The results of such supplementary studies must be available within 72 h.
The characteristic lesions associated with CBF leukaemia (i.e., CBFB::MYH11 and RUNX1::RUNX1T1) should be identified within 72 h of sample receipt. This can be undertaken by FISH, molecular characterisation or a rapid karyotype. It is important to note that cytogenetically cryptic CBFB rearrangements must be excluded by FISH or molecular characterisation where a diagnostic suspicion of CBF leukaemia persists.
Testing for KMT2A (MLL) rearrangement is essential, but less time critical than CBF, or FLT3, as it is less likely to impact initial therapy decisions. As KMT2A rearrangements may be cytogenetically cryptic,28 and are recognised as a disease defining entity in the updated WHO classification, KMT2A testing is mandatory for cases where no other DGA is identified. Given the well documented heterogeneity of KMT2A fusions, a gene partner agnostic approach such as “break-apart” FISH testing is essential. Supplementation by an RNA-based NGS fusion panel may be helpful. Where a KMT2A rearrangement is identified by a partner agnostic approach, it is essential for appropriate risk categorisation that further testing is undertaken;3 this may be by karyotype, metaphase FISH or molecular characterisation. With the continuing development of genomically derived disease classifications1, 2 expanded molecular profiling, for example through rapid whole genome sequencing or RNA-based NGS fusion panels, will play an increasingly important role in AML diagnosis.
Internal tandem duplications (ITD) and tyrosine kinase domain (TKD) driver variants in FLT3 have been shown to respond to FLT3 inhibitors and as such their rapid identification is critical. Although the FLT3-ITD allelic ratio (AR) is no longer required for assignment of ELN risk group, it is recommended that this is still reported if the assay is appropriately standardised and validated for this purpose,29 as AR provides additional prognostic information which may be valuable in some situations. Whilst rapid identification of the recurrent driver variants in exon 11 of NPM1 is not mandated, in practice they are often identified in tandem with FLT3 analyses for prognostic purposes and can also aid interpretation of cases of suspected APL without PML::RARA rearrangement as well as cases with morphological evidence of dysplasia.25
NGS panel testing for the identification of pathogenic variants within CEBPA, TP53, FLT3, IDH1, IDH2, ASXL1, BCOR, EZH2, RUNX1, SF3B1, SRSF2, STAG2, U2AF1, DNMT3a, WT1 and ZRSR2 is mandatory and will aid in using a genomic classification32 of AML and ELN 2022 risk stratification. There is no standard NGS panel in use by UK Genetics Laboratories; panel design, target enrichment techniques, and sequencing are available from a variety of commercial and in house methods. They must meet minimum standards of practice and requirements as defined in local or National testing algorithms, for example the National Genomic Test Directory (https://www.england.nhs.uk/publication/national-genomic-test-directories/) for services commissioned by NHS England, and remain flexible to incorporate changes in practice. NGS methods can have variable performance, particularly for detection of mutations in key genes that are difficult to sequence, such as CEBPA and quantification of FLT3 ITD. It is the responsibility of the testing laboratories to have robust NGS methods for the detection of typical mutations of mandatory targets or to provide alternative, quality assured single target tests. The majority of NGS panels available for use in AML will also contain a range of genes associated with other myeloid diagnoses and the reporting of these is considered desirable, but not mandatory at this time. In the future, rapid diagnostics for these and other abnormalities may be required for selection of upfront therapy, however at present this is only relevant within specific clinical trials and should be provided by the respective trials laboratory where needed.
It is important to recognise that driver variants identified by somatic-only testing may be of germline origin, and protocols to robustly identify and confirm such variants in high-actionability germline cancer predisposition genes (i.e., RUNX1, CEBPA, DDX41, ANKRD26, ETV6, GATA2) are essential (Table 5). Laboratories must have processes in place to identify and report potential germline findings30 in high-actionability genes from somatic only sequencing. Where a potential germline finding has been identified, a detailed clinical and family history is essential in determining whether to pursue further testing to confirm the aetiology of the variant. Should germline testing be indicated then a skin biopsy to obtain cultured skin fibroblasts will be required for further characterisation. Discussion and, depending upon local practice, referral of such cases to Clinical Genetics should be considered.
| Test name | Indication | TAT (days) |
|---|---|---|
| FISH PML::RARA [t(15;17)] | Suspicion of APL from morphology or flow | 1 |
| RT-PCR PML::RARA [t(15;17)] | Suspicion of APL from morphology or flow | 3 |
| MyeChild01 FISH panela | Children and young adults, if no other primary genetic changes | 7 |
| MLDS NGS panel (GATA 1) | Children with known trisomy 21 | 21 |
| Fanconi breakage testing | Suspected Fanconi anaemia pre-transplant | 14 |
| Inherited bone marrow failure syndrome panel | Suspected familial predisposition syndrome | 84 |
- a MyeChild01 FISH panel: t(5;11)(q35;p15.5)/NUP98::NSD1, t(7;12)(q36;p13)/MNX1::ETV6, inv (16)(p13.3q24.3)/CBFA2T3::GLIS2.
It is important to stress the identification of familial predisposition to haematological cancer, particularly to enable wider testing when considering transplantation from a related donor. A family history of MDS/acute leukaemia/aplastic anaemia, early onset of cancers of any type, or multiple close relatives with cancer should always be sought. In addition, a personal or family history of cytopenias, abnormal bleeding, skin/nail abnormalities, idiopathic liver disease, immune defects, atypical infections, lymphoedema, limb abnormalities or pulmonary fibrosis should be elicited. Index patients reporting this history should be referred to Clinical Genetics for counselling and expert advice.
Conversely, in patients with a clinical or family history suggestive of an AML predisposition syndrome or inherited bone marrow failure disorder, up-front germline testing may be warranted. Testing will typically be undertaken by large constitutional NGS panel analysis although, where there is a suspicion of Fanconi anaemia, then functional cytogenetic studies of mutagen (e.g., Diepoxybutane DEB, Mitomycin C MMC) sensitivity may be appropriate, with further characterisation of any positive findings by molecular studies to inform wider family studies.
Whole genome sequencing (WGS) is an emerging technique in UK clinical practice which at present may be used to supplement standard-of-care studies. WGS offers the potential to replace and enhance standard-of-care diagnostics and as WGS pathways embed and expand, and as the turnaround times for testing improve, it is likely that this technique will supplant some of the current testing modalities.
As these assays are RNA-based, it is essential that RNA is stored at diagnosis for an accurate baseline assessment, and that follow-up samples reach the molecular MRD laboratory within 2 days of sampling. Further recommendations on molecular MRD testing will become available in NHS England guidance documents in due course. Other molecular MRD monitoring techniques such as digital droplet PCR and NGS are currently under investigation and not yet recommended for routine clinical care.
Genetics recommendations
- Cytogenetic and molecular genetic analyses are critical at diagnosis and relapse
- Where indicated, PML::RARA testing must be completed within 24 hours of sample receipt
- Rapid identification of core binding factor leukaemia, FLT3 internal tandem duplication (ITD) and tyrosine kinase domain (TKD) mutations is essential
- A complete conventional cytogenetic analysis is required within 7 days of sample receipt
- Molecular MRD assessment should be performed for patients with an NPM1 mutation, CBFB::MYH11, RUNX1::RUNX1T1 and PML::RARA fusions, and considered for other fusion genes.
- Where a suspected germline finding in a cancer susceptibility gene is identified, it should be clearly highlighted in the genetic report.
ACKNOWLEDGEMENTS
The BSH Haematology Oncology task force members at the time of writing this good practice paper were Professor Barbara Bain, Dr Robert Sellers, Dr Gail Jones, Dr David Bloxham, Dr Mamta Garg, Dr Simon Stern, Dr Nilima Parry-Jones, Dr Guy Pratt, Dr Tracey Chan. The authors would like to thank them, the BSH Haematology Oncology sounding board, and the BSH guidelines committee for their support in preparing this good practice paper.
CONFLICT OF INTERESTS
The BSH paid the expenses incurred during the writing of this good practice paper. All authors have made a declaration of interests to the BSH and Task Force Chairs which may be viewed on request. PM has undertaken advisory board, educational. Grant or speakers fees with Pfizer, Jazz Pharmaceuticals, Astellas and Abbvie. SK: Advisory board: Astellas, Jazz, Servier, Abbvie, Novartis. Speakers fees: Astellas, Novartis, Jazz. Research funding: Novartis. AH: Advisory Board Novartis; Speakers' Bureau Gilead, Roche, Pfizer, Jazz, AbbVie; Data analysis CTI. SF: Speakers Bureau: Jazz, Novartis, Research Funding: Jazz, BMS, Advisory Board: Novartis, Neogenomics, IMPAAC. MC: Research funding from Cyclacel and Incyte; Advisory board member for Novartis, Incyte, Jazz, Servier, Pfizer. Honoraria: Astellas, Novartis, Jazz, Pfizer and Incyte.
REVIEW PROCESS
Members of the writing group will inform the writing group Chair if any new pertinent evidence becomes available that would alter the strength of the recommendations made in this document or render it obsolete. The document will be archived and removed from the BSH current guidelines website if it becomes obsolete. If new recommendations are made an addendum will be published on the BSH guidelines website (www.b-s-h.org.uk).
DISCLAIMER
While the advice and information in this guidance is believed to be true and accurate at the time of going to press, neither the authors, the BSH nor the publishers accept any legal responsibility for the content of this guidance.
APPENDIX A
A.1 2022 WHO classification acute myeloid Leukaemia1
APPENDIX B
B.1 2022 European Leukaemia net risk stratification of AML by genetics
| Genetic group | Subsets |
|---|---|
| Favourable |
t(8;21)(q22;q22); RUNX1::RUNX1T1 inv (16)(p13.1q22) or t(16;16)(p13.1;q22); CBFB::MYH11 Mutated NPM1 without FLT3-ITD bZIP in-frame mutated CEBPA |
|
Intermediate |
Mutated NPM1 with FLT3-ITD Wild-type NPM1 with FLT3-ITD t(9;11)(p21.3;q23.3)/MLLT3::KMT2A Cytogenetic and/or molecular abnormalities not classified as favourable or adverse |
| Adverse |
inv (3)(q21q26.2) or t(3;3)(q21;q26.2); GATA2, MECOM (EVI1) t(6;9)(p23;q34)/ DEK::NUP214 t(v;11)(q23.3)/KMT2A-rearranged t(9;22)(q34.1;q11.2)/ BCR::ABL1 −5 or del(5q); −7; −17/abn(17p) Complex karyotype (≥3 abnormalities) / monosomal karyotype Mutated ASXL1, BCOR, EZH2, RUNX1, SF3B1, SRSF2, STAG2, U2AF1 or ZRSR2 Mutated TP53 |
Note: NB Initial risk assignment for favourable/intermediate by genetics may change during the treatment based on MRD results.