Overview on Hereditary Spherocytosis Diagnosis
Funding: The authors received no specific funding for this work.
ABSTRACT
Introduction
Hereditary spherocytosis (HS) is a congenital haemolytic disorder, resulting from plasma membrane protein deficiency of red blood cells (RBCs). Typical pathological signs are anemia, jaundice, and splenomegaly; in newborns, jaundice is the main symptom.
Material and Methods
This study focused on the state of art about the HS diagnosis, from traditional to innovative methods, including diagnostic algorithms that can be applied for pediatric and adult patients, for different laboratory diagnostic levels.
Results
The first erythrocyte parameters used for HS diagnosis were the mean corpuscular hemoglobin concentration (MCHC), mean corpuscular volume (MCV), and red blood cell distribution width (RDW); nowadays new parameters are used in blood cell counter. Advia analyzers (Siemens Medical Solutions) supply the hyper-dense cell percentage (% Hyper), which reflects the red blood cells hyperchromia. Sysmex instruments (i.e. XT-4000i, XE-5000, XN-Series) provide the MicroR, that is the percentage of erythrocytes smaller than 60 fL, Hypo-He, which is the percentage of erythrocytes with a content of hemoglobin less than 17 pg and % Hyper-He, which represents the percentage of RBC with cellular hemoglobin content higher than 49 pg. CELL-DYN Sapphire (Abbott Diagnostics) introduced the HPR parameter (% HPR), which represents the erythrocytes with hemoglobin > 410 g/L. Beckman Coulter instruments supply the mean sphered corpuscular volume (MSCV), which is the average volume of all erythrocytes, including mature erythrocytes and reticulocytes. Other reference tests for screening and diagnosis of HS are the acidified glycerol lysis test (AGLT), the eosin-5-maleimide (EMA) binding test and genetic testing by next-generation sequencing.
Conclusions
The diagnostic workup of hereditary spherocytosis could be improved thanks to all the available tests, including new molecular tools. However, it requires synergy between clinicians and laboratory staff, evaluating clinical manifestations, all available data related to the disease and the prognosis to fill the diagnostic gaps in the near future.
1 Introduction
Hereditary spherocytosis (HS) is included among congenital hemolytic anemia. It is caused by plasma membrane protein deficiency, resulting in spherical-shaped red blood cells (RBCs), which are prone to hemolysis [1-3]. There is little data regarding the epidemiology of HS: in North America and Northern Europe the incidence is 1/5000 [4]. The prevalence of the disease above two areas is 1/2000–1/5000. The prevalence of HS in Europe is 1–5/10 000 [5], however, the disease is mostly common in Caucasians, whose prevalence is 1–2/5000, although by Kutter it is much higher due to the lack of symptoms in the majority of the cases [6]. In China, the prevalence of HS estimated by Wang et al. [7] was 1.27/100.000 in males and 1.49/100.000 in females. About 75% of cases present an autosomal dominant inheritance [8, 9].
1.1 Biochemical Abnormalities Associated With HS
The main cause of HS is based on erythrocyte membrane protein defects, with a resulting reduction in surface-to-volume ratio. To date, the main membrane protein mutations involve ankyrin-1, band 3, α, β-spectrin, and protein 4.2 [10]. RBCs thus become spheroidal and osmotically fragile cells, which are prone to be destroyed in the spleen [11]. According to the study of Mariani et al. [12], band 3 protein mutations were detected in approximately 54% of 300 European patients with HS. Park et al. [13] discovered that mutations in ankyrin protein are found in 52% of HS patients in South Korea.
1.2 Clinical Features
According to the “guidelines for the diagnosis and management of HS” [14], the patients are clinically classified as “mild,” “moderate,” or “severe”: the clinical severity of the disease is linked to the lower spectrin content. Typical pathological signs include anemia, jaundice, and splenomegaly. The degree of anemia is associated with spleen size and hemolysis. As for the last one, severe patients lack single membrane protein or have multiple protein mutations (commonly affecting band 3 and ankyrin), consequently more severe hemolytic anemia [15]. Splenectomy can help reduce symptoms, however, patients with severe HS remain anemic also postsplenectomy. Jaundice is commonly found in the first 2 days of life: it may be so serious that an exchange transfusion is required. However, it is not yet known whether it is linked to the severity of HS. In children and adults with HS, spleen enlargement can be observed, but other than helping in making diagnosis, it has little clinical significance.
1.3 Laboratory Investigations
The HS diagnosis is focused on laboratory data, above all red cell indices, erythrocyte morphology, and reticulocyte count, in addition to clinical features, physical examination, and family history. The amount of erythrocyte diseases is very large, such as acquired hemolytic anemia, hemoglobinopathies, and intra-erythrocyte enzyme deficiencies. For this reason, many screening and laboratory tests have been introduced to distinguish the different diseases and to rule out confounding blood pathologies. The main reference tests for screening and diagnosis of HS are complete blood count analysis, the eosine-5-maleimide (EMA) binding test, the acidified glycerol lysis test (AGLT), and sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE). Unfortunately, not all these tests are easy to perform. They often require specialized centers and highly qualified operators, and, above all, none of these tests, carried out individually, is able to diagnose all cases of HS [16, 17].
1.4 Complete Blood Count (CBC) Analysis
The oldest and most important erythrocyte indices used for HS diagnosis are the mean corpuscular volume (MCV), the mean corpuscular hemoglobin concentration (MCHC), and red blood cell distribution width (RDW) [18]. MCHC and RDW indices are increased in HS, MCHC could be normal in mild cases and elevated in moderate and severe ones. These findings can allow diagnosis with a good probability and interesting levels of sensitivity and specificity [19, 20]. At this time, many hematological analyzers provide additional erythrocyte markers, useful to the laboratory specialist to suspect the presence of spherocytes that, in the appropriate context, may lead to suspicion of HS diagnosis. Among them, the Advia analyzer (Siemens Medical Solutions Diagnostics, NY, USA) supplies a parameter obtained by a double-beam laser technology, that connects light scattering measurement from hemoglobin content (HC) and volume (V) per cell, obtaining a cytogram (V/HC) indicating the hyper-dense cell percentage (% Hyper): this parameter highlights the RBC hyperchromia [21]. Abbott Diagnostics (Abbott Diagnostics, Santa Clara, CA, USA) developed a new software for the Cell-Dyn Sapphire analyzer, which allowed the measurement of extended RBC and reticulocyte parameters, detecting hyperchromic RBC (HPR), which corresponds to erythrocytes with hemoglobin > 410 g/L, using a multi-angle light scatter technology [22] and correlates spherocytes with increased HPR.
Sysmex instruments (i.e., XT-4000i, XE-5000, XN-Series) introduced MicroR, which corresponds to the percentage of erythrocytes smaller than 60 fL and two other parameters, based on the mean HC of all the RBC analyzed in the reticulocyte channel: % Hypo-He, defined as the percentage of erythrocytes with a content of hemoglobin less than 17 pg and % Hyper-He, which represents the percentage of RBC with cellular HC higher than 49 pg [23]. On Sysmex analyzers spherocytes are characterized by an increased % Hyper-He and MicroR count, a decreased % Hypo-He count, and an increased MicroR/Hypo-He ratio. This is the consequence because the spherocytes are small, dense, and hyperchromic RBC and they have a reduced membrane surface area-to-volume ratio [24, 25]. Beckman Coulter instruments (Beckmann Coulter Inc., Fullerton, CA, USA) offer a new and original parameter, the MSCV, which is an artificial volume measurement count [26, 27]. The MSCV represents the average volume of all erythrocytes, both mature erythrocytes and reticulocytes, thanks to a mild swelling in the hypo-osmotic solution, used in the reticulocyte count [2]. Normally MSCV should be higher than MCV, in patients with HS, instead, MSCV is lower than MCV, due to the rigidity of the membrane and the consequent inability of the spherocytes to swell and expand their volume in hypo-osmotic solution. Low MSCV has been demonstrated to be a sensitive parameter for HS detection; one parameter that has proven to be very interesting is the difference between MCV and MSCV (MCV-MSCV), also known as delta MCV-MSCV. This calculation, when increased, has an even higher discriminatory value for HS detection [28, 29]. When the delta (MCV-MSCV) value is greater than 9.6 fL, HS could be suspected. For this reason, each laboratory should validate its own cutoff point, because different hematological analyzers cannot be compared.
1.5 Reticulocyte Count
Reticulocyte indices are very important for HS screening: the decrease in the surface-to-volume ratio is a characteristic that belongs to both reticulocytes and spherocytes. The reticulocyte parameters developed on the latest hematological analyzers are the absolute number of reticulocytes, the immature reticulocyte fraction (IRF), and mean reticulocyte volume (MRV or MCVr), which represent the average volume of all reticulocytes. A low MRV has been demonstrated to be a good parameter to discriminate between HS and non-HS subjects. However, it has a lower sensitivity and specificity than other reticulocyte indices [28]. Patients with HS are also characterized by a high reticulocyte count with a low immature reticulocyte fraction (IRF). The combination of reticulocyte count and immature reticulocyte fraction (Ret/IRF ratio) is another useful parameter for the screening of HS. Mullier et al. showed that mild cases of HS have a Ret/IRF ratio higher than 19, while severe cases of HS have a Ret/IRF ratio higher than 7.7 [30]. In the study of Lazarova et al., IRF compared to delta (MCV-MSCV) or MRV, proved effective diagnostic performances, lower specificity, lower positive predictive value, and likelihood ratio. Combining some parameters into diagnostic algorithms, such as MCV-MSCV > 10 with MRV-MSCV < 25, sensitivity and specificity have been improved [29].
1.6 Which Method Is Better?
Anne-Sophie Adam et al. [31] evaluated and compared the effectiveness of six published algorithms for HS screening. The study was based on the use of the UniCel DxH800 (Beckman Coulter) and the XN-9000 (Sysmex) analyzers, with the aim of determining the most suitable algorithm in daily clinical practice (Table 1). The reticulocyte parameters used on the DxH800 were MRV, IRF, and MSCV. On the XN-9000 were hypohemoglobinized erythrocytes, microcytic erythrocytes, and IRF. Regarding the Beckman Coulter analyzer parameters, the algorithm proposed by Liao et al. [32] achieved the best performances, with the correct identification of all HS patients tested (specificity 94.9%). On the other hand, the other two algorithms published by Lazarova et al. [26] and Nair et al. [29], had poorer results. The three algorithms applied on the Sysmex instruments, that is, the algorithms published by Mullier et al. [30], Persjin et al. [33], and Bobee et al. [24] showed similar performances to the ones obtained with the Beckman Coulter analyzer.
| Author | Instrument | Algorithm (Ret μL) (Hb g/L) (MicroR %) | Sensitivity (%) | Specificity (%) | ||
|---|---|---|---|---|---|---|
| Mullier et al. (2011) [30] | Sysmex XE5000 | Ret ≥ 80 000 e Ret/IRF > 7.7 | 100.0 | 99.3 | ||
| Hb > 120 Ret/IRF ≥ 19 | 80 ≤ Hb ≤ 120 MicroR ≥ 3.5 e MicroR/Hypo-He ≥ 2.5 | Hb < 80 MicroR ≥ 3.5 e MicroR/Hypo-He ≥ 2 | ||||
| Trait and Mild HS | Moderate HS | Severe Hs | ||||
| Persijn et al. (2012) [33] | Sysmex XE5000 | Ret ≥ 100 000 e Ret/IRF > 7.7 | 84.0 | 99.0 | ||
| Hb > 120 Ret/IRF ≥ 19 | 80 ≤ Hb ≤ 120 MicroR ≥ 2.6 e MicroR/Hypo-He ≥ 2.5 | Hb < 80 MicroR ≥ 2.6 e MicroR/Hypo-He ≥ 2 | ||||
| Trait and mild HS | Moderate HS | Severe Hs | ||||
| Bobee et al. (2018) [24] | Sysmex XE5000 | Ret > 80 000 and Ret/IRF > 9.1 and MicroR (if Hb < 120) > 2.2 and MicroR/Hypo-HE (if Hb > 120) ≥ 3.5 | 100.0 | 92.1 | ||
| Lazarova et al. (2014) [26] | Beckman Coulter UniCel DxH800 | (MCV-MSCV-MRV fL) | ||||
| MCV-MSCV > 10.4 and/or MSCV < 70.2 and/or MRV < 96.7 | 100 | 74 | ||||
| 92 | 90 | |||||
| 100 | 88 | |||||
| Nair et al. (2015) [29] | Beckman Coulter LH755 | MCV-MSCV > 10 and MRV-MSCV < 25 | 84.2 | 94.7 | ||
| Liao et al. (2019) [32] | Beckman Coulter LH780 | MSCV-MCV < 0.6 | 95.5 | 94.9 | ||
| Rooney et al. (2015) [22] | Abbott Cell-Dyn Sapphire | HPR% | 96.4 | 99.1 | ||
- Abbreviations: Hb, hemoglobin concentration; HPR%, hyperchromic RBC; Hypo-He, percentage of erythrocytes with a content of hemoglobinaemoglobin less than 17 pg; IRF, immature reticulocyte fraction; MCV, mean corpuscular volume of erythrocytes; MicroR, percentage of erythrocytes smaller than 60 fL; MRV, mean reticulocyte volume; MSCV, mean sphered corpuscular volume of erythrocytes; Ret, reticulocyte count.
On the other hand, Rooney et al. [22] tested the hyperchromic RBC (HPR) in pediatric patients using the Cell-Dyn Sapphire analyzer: the ROC analysis showed that HPR had high sensitivity (96.4%) and specificity (99.1%), with an optimal cutoff value of 4.9% [22].
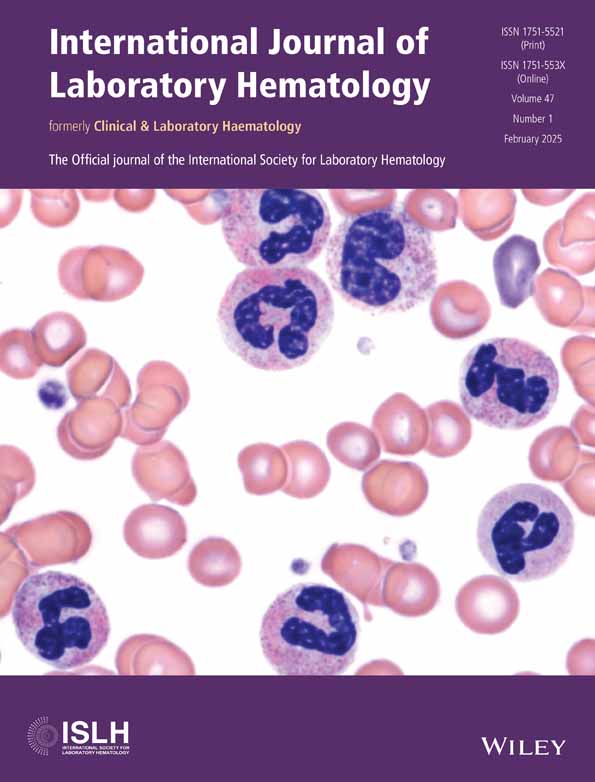
1.7 Morphology Analysis
According to the first “guidelines for the diagnosis and management of HS” [14] well-defined cases characterized by clinical details, such as the presence of spherocytes and reticulocytosis or a negative direct antiglobulin test (DAT), will support the diagnosis of HS. When there is no family history, an important differential diagnosis is autoimmune hemolytic anemia (AIHA), which is rare in children. AIHA can sometimes be excluded by a negative DAT. Nonetheless, the absence of spherocytes on the blood smear, or normal red cell indices with typical reticulocyte count, then a ‘carrier’ condition should be considered. If the morphology is atypical, other membrane abnormalities must be considered, especially, for congenital dyserythropoietic anemia type II (CDAII).
1.8 Osmotic Fragility (OFT) Test
OFT is a semiquantitative test that assesses erythrocyte hemolysis as a consequence of hypotonic solutions of sodium chloride (NaCl) treatment. Spherocytes hemolyze after exposure to NaCl, because of their lower osmotic resistance compared to normal RBC. Positive results are reported in many diseases such as HS, hereditary elliptocytosis, and autoimmune hemolytic anemia [34]. Shim et al. [35] compared HS patients with non-HS controls. In patients with HS, the OFT showed a diagnostic sensitivity and specificity of 66% and 81.8%, respectively. Overall, a normal result cannot rule out the diagnosis of HS, this condition represents 10%–20% of HS cases.
In the same way, a newborn could be considered as a false negative due to the high level of fetal hemoglobin (HbF), which gives erythrocytes more resistance to hemolysis.
1.9 AGLT
The AGLT is based on the affinity of glycerol and membrane lipids for a hypotonic salt buffer, that chemically reacts with erythrocyte membrane, causing hemolysis of RBC. As cell lysis increases, the absorbance of the solution declines gradually to half the initial absorbance level [36]. Even if the AGLT test has a high sensitivity, it has reduced specificity, and it is time-consuming.
1.10 EMA
This is a flow cytometric test, which is based on the binding of the Eosin-5′-maleimide to band 3 protein. EMA provides quantitative results: it is interpreted as positive for HS when the grade of fluorescence is > 21%, negative if fluorescence is < 16% [37, 38], and equivocal if the percentage is included between 16% and 21% [39]. EMA has a high sensitivity (92.7%–96.6%) and specificity (99.1%) for HS diagnosis. EMA test is considered the most accurate screening test, with a relatively short time-around-time (TAT), high sensitivity, economical, and feasibility also in laboratories furnished with a basic flow cytometer. Furthermore, the EMA test can discriminate between different red cell populations, so that the results are not skewed in patients undergoing transfusion [40].
1.11 Plasma Membrane Protein Electrophoresis
Sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE), different from other tests, consents to the qualitative and quantitative identification of abnormal plasma membrane protein content. Differently from EMA or the OFT test, which are much more common [16], the SDS technique can only be performed in specialized diagnostic centers and is time-consuming. Unfortunately, the SDS test in 10%–20% of cases, could not detect deficient plasma membrane.
1.12 Genetic Testing
The genetic expression study of HS is used in association with the standard screening tests in order to enhance the reliability of HS diagnosis. Actually, some laboratories use the high-resolution melting curve technique, even if it has some limitations, such as poor identification of A/T or G/C base changes. For this reason, it was partially replaced by next-generation sequencing, which is the modern technology for genetic screening and diagnosis. The latter is a time- and cost-effective technology, characterized by high throughput and with appropriate phenotyping, which significantly increases the sensitivity (from 70% to 100%) [41]. In order to sequence and to screen potential variants deletion and/or duplication analysis at once, an NGS panel targeting ANK1, SPTB, SLC4A1, SPTA1, and EPB42 gene has been created: ANK1, SLC4A1, or SPTB mutations are common in patients with an autosomal dominant profile for HS [3].
The last guidelines suggest the use of genetic testing in association with other screening tests, when the diagnosis of HS is difficult, especially in the presence of mild clinical symptoms [42].
This is applied in a particular way to estimate the disease development, treatment options (splenectomy or not), and most of all, to allow genetic counseling for patients and their families [43]. In addition, genotyping is also useful to individuate a recessive inheritance or de novo variant, especially in HS cases without a clear family history. Finally, genotyping is useful in conditions of suspected HS, also with markedly different phenotypes: as it can be possible to see in cases of coexistent conditions that could decrease the severity of the HS [44].
1.13 Diagnostic Protocol for HS
- when the clinical appearance is more severe than the RBC morphology;
- when the red cell morphology is more severe than the one observed in family history;
- in case of the uncertainty of the diagnosis before the splenectomy.
The last update, published in 2021 [42], suggests a simple protocol for the diagnosis of HS, with the addition of some tests, such as MRV and MSCV. Furthermore, it takes into consideration symptoms, family history, diagnostic tests for hemolytic anemia, genetic testing, and other laboratory surrogate tests.
1.13.1 Screening Tests
- Hb level in trait form is normal; mild 110–150 g/L; moderate 80–120 g/L; severe 60–80 g/L.
- Reticulocyte count in trait form is < 3%; in mild cases 3%–6%; moderate > 6%; severe: > 10%.
- MCHC > 355 g/L is used as the cutoff for HS diagnosis.
- High number of spherocytes.
- Total serum bilirubin increased, especially for unconjugated bilirubin.
- MRV is decreased (cutoff: ≤ 95.77 fL); MSCV < MCV.
Differently from the previous guidelines, the last one suggests the use of analytical methods, such as OFT, AGLT, Coombs test, and G6PD level determination, in addition to genetic testing. On the other hand, ICSH proposed an algorithm in case of HS suspicion [2]. To verify the hemolysis, RDW-CV and parameters obtained from the reticulocyte channel are suggested. In order to analyze the presence of spherocytes or other morphological abnormalities, a blood smear is performed. If the HS diagnosis is still suspicious, cryo-hemolysis and EMA tests are suggested. In this case, there are two possibilities. Both negative tests: no further testing is required. Positive or doubtful results: the ektacytometry test is conducted.
Furthermore, if the patient's anamnesis is typical for HS, the diagnosis can be preserved. In case of doubtful anamnesis, SDS-PAGE is performed to exclude CDA II, to confirm the diagnosis of HS, and to determine the protein mutation. Molecular analysis is only performed in cases of chronic transfusion or mismatch between clinical profile and analytical results.
1.14 Making the Diagnosis of HS in a Newborn
About 65% of newborns with HS have a parent with the same pathology [45]. The clinical profile of HS through the perinatal period varies from severe fetal anemia with hydrops fetalis to the absence of symptoms. In newborns, jaundice is the most common symptom [46]. Approximately in one-third of newborns with HS, spherocytes are not detected in the blood smear, but pyknocytes: distorted densely stained red cells. According to the guidelines for the diagnosis and management of hereditary spherocytosis, in case of suspected HS [3], in newborns without symptoms, analytical tests can be rescheduled until the sixth month of age or later, as the morphology could be less confusing. Typically, a newborn with HS presents low MCV and elevated MCHC. New studies demonstrate that when MCHC > 360 g/dL in newborns, it suggests the presence of the disease (82% sensitivity and 98% specificity) [46]. Based on this data, the HS ratio in the neonatal period could be calculated by dividing the MCHC by the MCV. According to a recent review, when the HS ratio > 0.36 is predictive for identifying the disease, with 97% sensitivity and > 99% specificity [47]. HS could be suspected when the HS ratio intermediate [38, 39] or normal (< 35) is present. Using this ratio, an overlap may occur, whereby it is possible to differentiate HS newborns from healthy ones, through additional tests, such as elution of anti-A or anti-B from neonatal erythrocytes or indirect Coombs test. Since the HS diagnosis may be still uncertain, EMA binding or OFT testing could be performed [48]. Sequencing of the main genes can be done as a confirmatory test [49]. In this scenario, evaluating a newborn for HS, when a parent is known to have HS, according to the American Academy of Pediatrics' guidelines [50], it is important to treat the newborn as if they have HS, starting with the evaluation during the birth hospitalization. Among the exams, peripheral smear examination and a reticulocyte count are recommended, as well as bilirubin monitoring at birth and within 24 h before the hospital discharge.
Differently in the case of a jaundiced newborn with HS, whose parents are healthy, there is no need to wait for anemization to start the evaluation. However, in the case of hemolytic jaundice, it could be useful to perform a complete blood cell count with peripheral blood smear, blood type of mother and infant, DAT, reticulocyte count, and glucose-6-phosphate dehydrogenase deficiency testing. If the diagnosis of HS is doubtful, EMA binding or OFT testing could be performed or additional diagnostic testing, by NGS or a hematology consultant.
1.15 Confounding Factors in HS Diagnosis
- heterogeneous clinical manifestations of HS;
- the sensitivity or specificity of some parameter, such as MCHC, or diagnostic tests, such as OFT or red cell morphology;
- insufficient knowledge of HS.
Several common confounders include vitamin/iron deficiency, and the coexistence of other diseases, such as mild myelodysplasia in advanced age, which could hinder bone marrow compensation. Likewise, the presence of hemolysis associated with mechanical injury, toxic agents, and infections, which could be found in healthy subjects and many other hematologic diseases should be considered [51, 52]. Cases of HS misdiagnosis were reported by Deng et al. [53]. Overall, confounding factors should be taken into consideration, keeping an open-minded view when analyzing different pathological conditions characterized by hemolysis.
2 Conclusions
The HS diagnosis may be challenging due to the need for specialized tests and staff, including the symptom heterogeneity, which overall could cause a delayed diagnosis, misdiagnosis, or inappropriate therapies. Currently, HS diagnosis could be improved, thanks to all the new and traditional available tests. The characteristic morphology of spherocytes, consequently the abnormal concentration of hemoglobin, and the typical surface-to-volume ratio have prompted the technology to find methods to accurately measure these features. The first parameters used in the diagnosis of HS were MCHC and RDW, together with reticulocyte count and IRF. MCHC and RDW indices are increased in HS, particularly MCHC could be normal in mild cases and elevated in moderate and severe ones, reaching good levels of sensitivity and specificity. Regarding reticulocyte parameters, patients with HS are characterized by a high reticulocyte count with a low IRF: the combination of reticulocyte count and immature reticulocyte fraction (Ret/IRF ratio) is a useful parameter for the screening of HS. Some instruments have introduced innovative parameters, which are altered in the HS, such as the MSCV and the associated delta MCV-MSCV: in case delta MCV-MSCV > 10 there are good specificity and sensibility. In other cases, the great knowledge of physical principles has allowed us to discover new systems for correlating standard parameters and finding new strategies, such as the hyperchromic RBC (HPR) measurement, based on multi-angle laser scatter flow cytometry. Other technological systems have exploited the characteristic of erythrocytes that in HS are small, dense, and hyperchromic. Some authors found a very good statistical correlation with the diagnosis of HS, relating erythrocytes smaller than 60 fL (MicroR) to erythrocytes with hemoglobin concentration below 17 pg (Hypo-HE). Furthermore, an EMA binding assay or OF test allows for confirming or rejecting the presence of the disease. In the same way, further defects affecting RBC, such as acquired hemolytic anemia, hemoglobinopathies, and intra-erythrocyte enzyme deficiencies, are identified in the laboratory with all the available technologies and methods, from morphology to molecular biology, allowing the successful identification of individual atypical erythrocyte subset. However, the pathway of HS diagnosis, as well as other defects, primarily needs the synergy between clinicians and laboratory staff, evaluating clinical manifestations, all available data linked to the disease, and the prognosis. Furthermore, the availability of new molecular tools, such as NGS, could fill the diagnostic gaps in the near future, thus giving more value to genetic counseling, which is most in demand by affected families.
Author Contributions
The authors takes full responsibility for this article.
Acknowledgments
I would like to thank the SIPMeL Haematology Study Group for their trust, humanity, and patience in believing in this paper, through their constant support and their important skills, the result of decades of experience.
Ethics Statement
The authors have nothing to report.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data and information used for the drafting of this paper are available on request, writing to Dr. Alessandro Polizzi at Operative Unit of Clinical Pathology of “R. Guzzardi” Hospital in Vittoria, A.S.P of Ragusa.